Lymphoma—A Cancer That Touches Every Region
Lymphoma is the most common blood cancer worldwide, affecting both adults and children. It arises from lymphocytes—immune system cells, also called white blood cells—that grow uncontrollably. Lymphoma can develop in lymph nodes, the spleen, the thymus, bone marrow, and digestive organs, anywhere where lymph tissue exists.
Globally, the burden of lymphoma is on the rise. Every year, hundreds of thousands are diagnosed, with some regions—including parts of Africa, South Asia, and the MENA communities—seeing the sharpest increases in cases and deaths.
Lymphoma is the most common blood cancer worldwide, affecting both adults and children. It arises from lymphocytes—immune system cells, also called white blood cells—that grow uncontrollably. Lymphoma can develop in lymph nodes, the spleen, the thymus, bone marrow, and digestive organs, anywhere where lymph tissue exists.
Globally, the burden of lymphoma is on the rise. Every year, hundreds of thousands are diagnosed, with some regions—including parts of Africa, South Asia, and the MENA communities—seeing the sharpest increases in cases and deaths.
What Is The Lymphatic System?
Lymphoma is the most common blood cancer worldwide, affecting both adults and children. It arises from lymphocytes—immune system cells, also called white blood cells—that grow uncontrollably. Lymphoma can develop in lymph nodes, the spleen, the thymus, bone marrow, and digestive organs, anywhere where lymph tissue exists.
Globally, the burden of lymphoma is on the rise. Every year, hundreds of thousands are diagnosed, with some regions—including parts of Africa, South Asia, and the MENA communities—seeing the sharpest increases in cases and deaths.
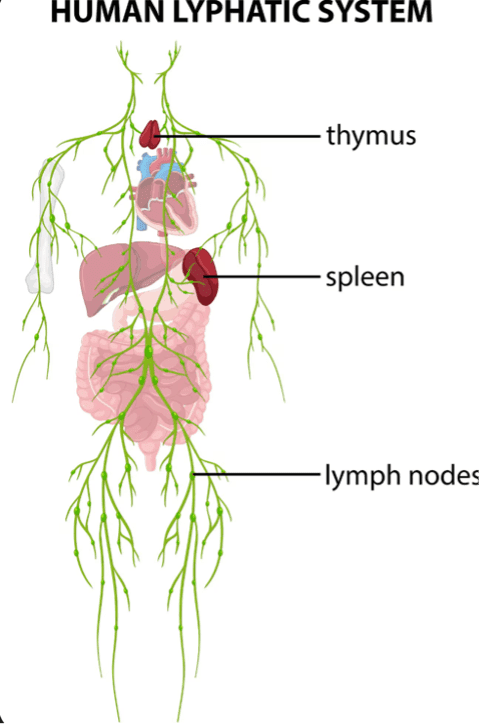
Lymphoma is the most common blood cancer worldwide, affecting both adults and children. It arises from lymphocytes—immune system cells, also called white blood cells—that grow uncontrollably. Lymphoma can develop in lymph nodes, the spleen, the thymus, bone marrow, and digestive organs, anywhere where lymph tissue exists.
Globally, the burden of lymphoma is on the rise. Every year, hundreds of thousands are diagnosed, with some regions—including parts of Africa, South Asia, and the MENA communities—seeing the sharpest increases in cases and deaths.
Lymphoma—When Life Changes Unexpectedly
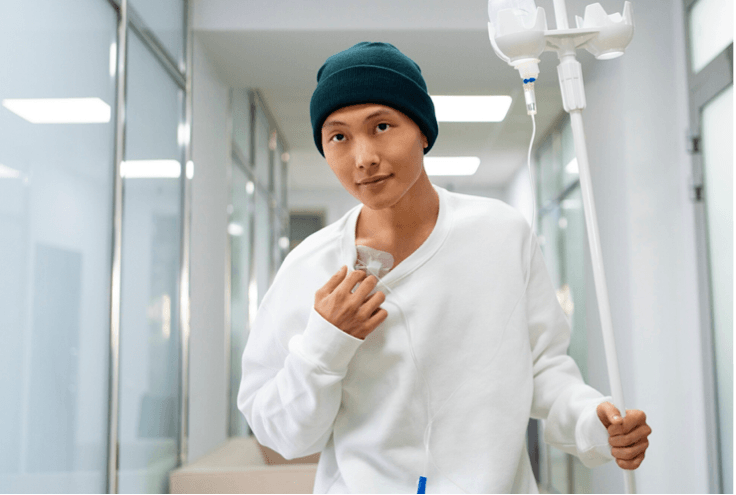
Lymphoma often enters a person’s life without warning—a painless lump appears in the neck or armpit, or fatigue lingers day after day. For many, the time before a clear diagnosis is full of vague symptoms and the feeling something is just wrong.
Once the word “lymphoma” is spoken, emotions run the spectrum—fear, relief at finally knowing what’s wrong, and immediate questions about treatment and family. It is important now to know about lymphoma, what is coming up, which therapy is to choose, what does it mean to the daily life – and what will be the outcome?
Let us give you the KnowHow to understand lymphoma, deal with the diagnosis, and make the right choices for a treatment you are confident with, and you can support the therapy for its best outcome.
What Is Lymphoma? Understanding This Common Blood Cancer
If you have lymphoma, your lymphocytes divide in an abnormal way, or they do not die after their usual life span. These abnormal lymphocytes often don´t function well, and they are overgrowing the healthy lymphocytes.
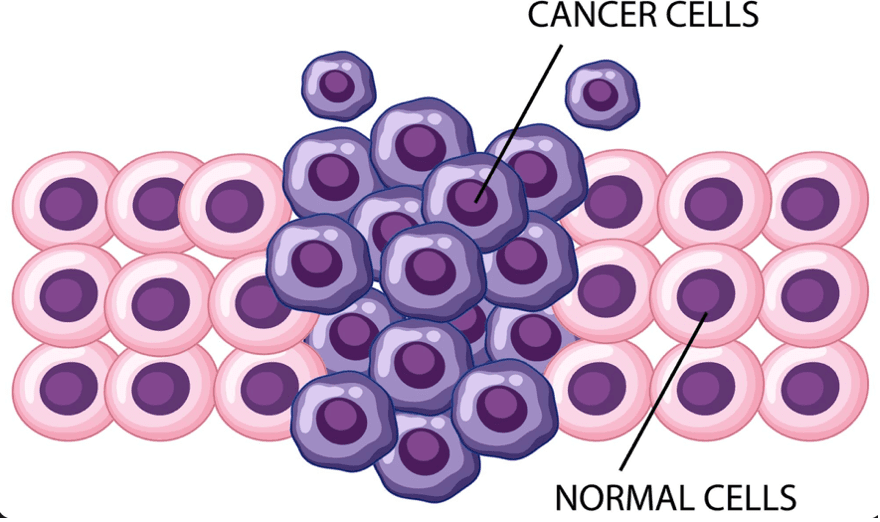
When these cells grow uncontrollably, lymphoma can develop anywhere in the lymphatic system—such as lymph nodes, the spleen, bone marrow, and other organs. The two broad types are non-Hodgkin lymphoma (NHL), the more common worldwide, and Hodgkin lymphoma (HL), which accounts for fewer cases but has distinct characteristics. Hodgkin’s lymphoma was named after Dr. Thomas Hodgkin who first recognized it in 1832. The cancer cells in Hodgkin’s and Non-Hodgkin’s disease look different under a microscope and therefore can be distinguished by histopathology and molecular pathology.
Lymphoma affects people across age groups, including children, adolescents, and adults. In the United Arab Emirates, the most recent available data (Globocan/IARC and UAE Cancer Registry) estimates approximately 95 new diagnoses for Hodgkin lymphoma and about 398 new cases for non-Hodgkin lymphoma every year.
Symptoms Of Lymphoma: What To Watch For
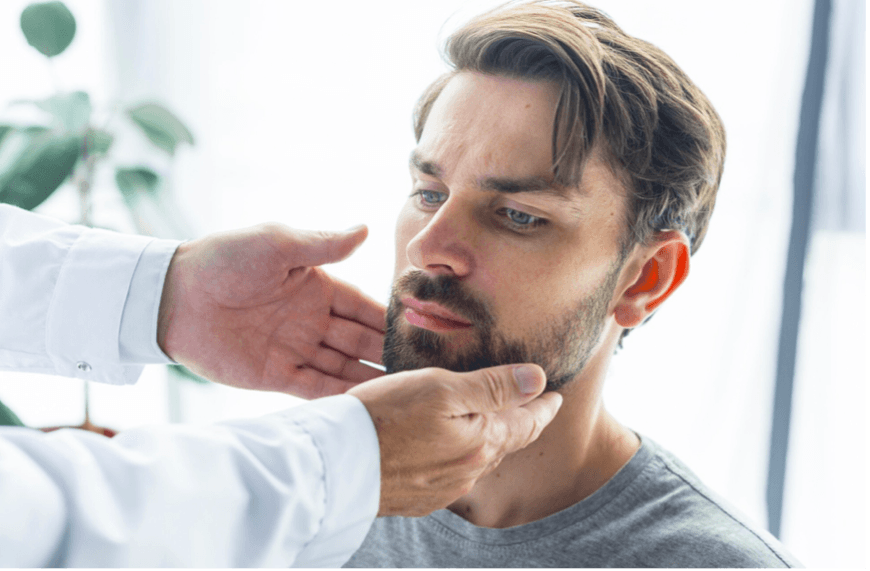
Early symptoms of lymphoma are often subtle and therefore either ignored in a busy daily life or mistaken for other illnesses. The most important sign you should watch for is painless swelling of lymph nodes in areas like the neck, armpits, or groin. While swelling of lymph nodes is normal when they combat germs, for example after an injury, an inflamed tooth, or an infection, these nodes often are noticed by rapid welling and discomfort.
Other symptoms include:
- an unexplained high fever that lasts longer than two days
- drenching night sweats
- unexplained weight loss of 10% or more of your total body weight over six months
- feeling much more tired than usual for at least several days (fatigue).
- itchy skin (pruritus), especially after drinking alcohol or taking a bath
- belly (abdominal) pain or swelling that doesn’t go away
- chest pain, and shortness of breath could be a sign of Hodgkin lymphoma in lungs or of a large mass in the chest
Doctors call fever, unintended weight loss and drenching night sweats associated with lymphoma “B symptoms.” The presence or absence of these B symptoms helps to determine the outcome and plan treatments.
It is important to seek medical advice when you recognize such signs persisting for several weeks.
What Causes Lymphoma? Risk Factors Explained
In most cases, the exact cause of lymphoma is unknown. However, research points to several risk factors linked to its development. In some cases, they are restricted to certain types of lymphomas, read also What Causes Hodgkin Lymphoma? Know The Risk Factors. and What Are Risk Factors of Non-Hodgkin Lymphomas?
- viral infections, like Epstein-Barr virus and HIV,
- a weakened immune system (due to diseases, medications, or genetic predisposition)
- exposure to environmental toxins such as pesticides or industrial chemicals
- lifestyle elements like smoking
- a family history of lymphoma
Most people diagnosed with lymphoma do not have identifiable risk factors.
How Is Lymphoma Diagnosed and Staged?
A diagnosis is confirmed through a biopsy. Tissue from an enlarged lymph node or affected site is surgically removed and examined microscopically and in a molecular pathology laboratory.
Blood and urine tests support the diagnosis by looking for organ involvement.
Imaging technologies, such as CT scans, PET scans, and MRI, provide detailed assessment of lymphoma location and spread.
In some cases, bone marrow examination is needed.
The results of these investigations allow specialized doctors (haematology and oncology) to stage lymphoma. Staging describes the extent of the cancer disease and tells how far it has spread. Accurate staging and characterization of the lymphoma type is critical to guide treatment, allow personalized care, and helps predict outcomes.
What Is Hodgkin Lymphoma?
There are 4 classic Hodgkin lymphoma subtypes:
Nodular sclerosis Hodgkin lymphoma. This is the most common classic Hodgkin lymphoma subtype. It often affects young adults, especially females. It typically affects lymph nodes in the central part of the chest.
Mixed cellularity Hodgkin lymphoma. This subtype typically affects people in their 60s. It sometimes develops in the belly (abdomen).
Lymphocyte-rich classic Hodgkin lymphoma. This Hodgkin lymphoma subtype affects about 6% of people with Hodgkin lymphoma. It’s more common in males.
Lymphocyte-depleted Hodgkin lymphoma. This subtype only affects about 1% of people with Hodgkin lymphoma. It’s most common in people who are older than 60 years and people who have HIV/AIDS.
How Common Is Hodgkin Lymphoma?
Hodgkin lymphoma is rare, affecting about 3 in 100,000 people each year globally and around 2 in 100,000 people in the UAE. While this makes it a rare disease, Hodgkin lymphomas are the most common cancers in teens between 15 and 19 and young adults.
What Causes Hodgkin Lymphoma? Know The Risk Factors.
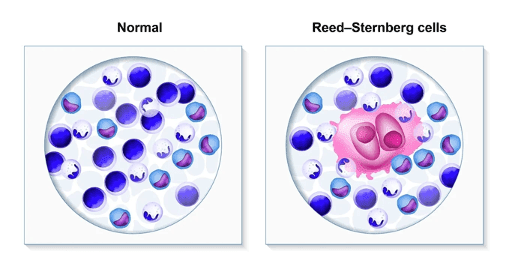
Hodgkin lymphomas form when B-cell lymphocytes develop genetic changes. These changes (mutations) are acquired. This means you develop them during your lifetime instead of being born with them.
When B-cells mutate, they create larger-than-normal cancerous cells called Reed-Sternberg cells. They produce cytokines, substances that attract normal cells to lymph nodes that contain the abnormal cells. These normal cells release substances that make the Reed-Sternberg cells grow. The result is swollen lymph nodes.
The cancer can spread through the lymphatic system to other lymph organs, like thymus and spleen. It can spread to lymph tissue throughout the body. Rarely, it can involve other organs like your lungs, liver and bone marrow (the production site of blood cells).
Healthcare providers have identified factors that may increase your risk of developing Hodgkin lymphoma, including:
Age: You’re more likely to develop this condition if you’re between 20 and 39 years old or older than 65.
Gender: Males are more likely to develop Hodgkin lymphoma. The exception is nodular sclerosis, a classic Hodgkin lymphoma subtype that’s more common in females.
Family medical history: You have a slightly increased chance of developing the condition if you have biological siblings or parents with Hodgkin lymphoma.
Having an organ transplant: If you had an organ transplant, you need to take antirejection medications that suppress your immune system. That increases your risk of developing lymphoma.
Having certain viruses: Having HIV, human T-lymphotropic virus type 1 or Epstein-Barr virus may increase your risk of developing Hodgkin lymphoma.
What Are The Stages Of Hodgkin Lymphoma?
Cancer staging helps doctors determine how advanced the cancer is, how quickly it may spread and what treatments may work best. Here are the stages for Hodgkin lymphoma:
Stage I. There are cancer cells in one lymph node area or lymphoid organ (like your thymus, spleen or bone marrow). Or there’s lymphoma in just one area of a single organ outside of your lymph system.
Stage II. There are cancer cells in two or more groups of lymph nodes on the same side of your diaphragm (may also affect other lymph nodes near your diaphragm).
Stage III. Lymph node areas on both sides of your diaphragm contain lymphoma cells, or there are cancer cells in lymph nodes above your diaphragm and in your spleen.
Stage IV. There’s lymphoma in at least one organ outside of your lymph system, such as your liver, lung or bone marrow.
Providers also use labels like “favorable” and “unfavorable” to classify Hodgkin lymphomas based on whether they’re likely to respond well to treatment and stay in remission (no signs or symptoms of cancer).
How is Hodgkin lymphoma treated?
Doctors use different treatment approaches for Hodgkin lymphomas depending on the stage of the cancer. These treatments either kill cancer cells or keep them from dividing. Treatment options include:
Chemotherapy. This common Hodgkin lymphoma treatment uses one or a combination of drugs to kill cancer cells or keep them from multiplying.
Radiation therapy. This therapy uses high-powered energy beams to kill cancer cells in affected lymph nodes or areas of cancer spread. It’s often used with chemotherapy in early-stage Hodgkin lymphoma treatment.
Immunotherapy. This treatment boosts the body’s immune system, so it’s better at identifying and destroying cancer cells. Checkpoint inhibitors are an important immunotherapy treatment for Hodgkin lymphoma.
Targeted therapy. Targeted therapy uses medication or other substances to attack cancer cells with specific characteristics. This treatment uses lab-created antibodies, which can find the cancer cells. As a chemotherapy drug is attached to the antibodies, they can destroy the cancer cells.
Chemotherapy with stem cell transplantation. This treatment may be an option when Hodgkin lymphoma has relapsed (come back after remission) or isn’t responding to treatment.
Each treatment has different side effects. Ask your healthcare provider about potential side effects before treatment. They’ll help you weigh the potential benefits of treatment against the possibility of side effects.
What Is the Outlook of Hodgkin Lymphoma?
Healthcare providers consider Hodgkin lymphoma to be a treatable and highly curable cancer. Your outlook will depend on the stage and other factors that your healthcare provider can discuss with you. That said, there are times when treatment doesn’t work or the cancer comes back.
In this situation, there is still the option of a palliative care: when a cure is not possible, there are treatments which help to slow down the progression of the cancer grow, reduce and ease symptoms, and supports life quality.
What Is Non-Hodgkin Lymphoma?
With non-Hodgkin lymphoma, genes inside B lymphocytes (B-cells) or T lymphocytes (T- cells) change (mutate) at some point in your lifetime. The abnormal lymphoma cells usually form in your lymph nodes and form tumors. But they can also be in other lymph system organs, like your thymus or spleen, or lymph tissue in other places. Without treatment, non-Hodgkin lymphoma can spread.
People with non-Hodgkin lymphoma are living longer than ever, thanks to new treatments. In some cases, treatments cure the condition. If cure is not possible, the goal of treatment is to put the disease into remission (no signs or symptoms of cancer) for as long as possible.
Types Of Non-Hodgkin Lymphoma
There are more than 70 subtypes of non-Hodgkin lymphoma.
Doctors classify them based on the type of lymphocyte affected:
B-cell lymphoma. These cancers arise from B-cells. B-cells make antibodies that fight infection-causing germs. B-cell lymphomas account for about 85% of all NHL diagnoses.
T-cell lymphoma. These cancers arise from T-cells. T-cells target germs and other foreign cells and help B-cells make antibodies.
Providers classify B-cell and T-cell lymphomas as either aggressive or indolent (slow-growing). Aggressive non-Hodgkin lymphomas spread faster than indolent non-Hodgkin lymphomas. Aggressive NHL often requires more intensive treatment.

What Are Risk Factors of Non-Hodgkin Lymphomas?
There are several risk factors linked to non-Hodgkin lymphoma (NHL). A risk factor is a trait, activity or condition that increases your risk of developing a disease. For example, people more likely to get diagnosed with NHL are:
Age: You’re more likely to develop this condition if you’re older than 60.
Gender: Males are more likely to develop non-Hodgkin lymphoma.
Family medical history: Your risk may be greater if you have a parent, sibling or child with lymphoma or other blood cancer.
Autoimmune diseases. People with inflammatory bowel disease (IBD), rheumatoid arthritis, psoriasis or other rheumatologic conditions may have an increased risk of developing NHL.
Having an organ transplant: If you had an organ transplant, you need to take antirejection medications that suppress your immune system. That increases your risk of developing lymphoma.
Infections. Bacterial and viral infections that have been linked to non-Hodgkin lymphoma include H. pylori infection (MALT lymphoma of the stomach), human T-lymphotropic virus Type I, Hepatitis C and Epstein-Barr virus.
Exposure to pesticides. Some research shows that people exposed to high levels of weed killers and insecticides may have a slightly increased risk of non-Hodgkin lymphoma.
Previous cancer treatment. Some treatments, such as chemotherapy drugs or CAR-T cell therapy, used to treat other types of cancer, including other blood cancers, might increase the chance of developing lymphoma in the future. The same is true to exposure to radiation, including radiotherapy for other cancers. However, most people who’ve been treated for another cancer do not develop lymphoma.
Stages Of Non-Hodgkin Lymphoma
The stages of non-Hodgkin lymphoma are:
Stage I. One lymph node area or lymphoid organ contains cancer cells. Or there’s lymphoma in one area of a single organ outside of your lymph system.
Stage II. There’s lymphoma in two or more groups of lymph nodes on the same side of (or near) your diaphragm.
Stage III. There are cancer cells in lymph node areas both above and below your diaphragm or in the lymph nodes above your diaphragm and in your spleen.
Stage IV. At least one organ outside your lymph system, like your liver or lung, contains widespread lymphoma.
How Is Non-Hodgkin Lymphoma Treated?
There are several types of treatment for non-Hodgkin lymphoma. The treatment you’ll need depends on factors like the type of NHL, the cancer stage and your overall health.
Indolent non-Hodgkin lymphoma types are growing very slowly. What is good news means on the other hand, that indolent non-Hodgkin lymphomas are currently thought to be not curable. Aggressive non-Hodgkin lymphomas consist of fast dividing cancer cells which gives chemotherapy a better chance to effectively combat these cells.
Treatments include:
Active surveillance. If you have an indolent (slow growing) non-Hodgkin lymphoma and aren’t experiencing symptoms, your doctor may hold off on treatment. This is called active surveillance, or watchful waiting. Doctors monitor your health, so they’re ready to start treatment as soon as you have symptoms. Don´t be worried to miss anything if you don´t start early with the treatment. Overall, this strategy is currently the best option for your overall health and outcome.
Chemotherapy. Chemotherapy uses drugs to attack cancer cells throughout your body. It’s the most common NHL treatment. You may get chemo alone or alongside other treatments.
Targeted therapy. These treatments work on specific characteristics in cancer cells to destroy them. Monoclonal antibody therapy is a common targeted therapy treatment for NHL.
Immunotherapy. This treatment boosts your body’s immune system, so it’s better at destroying cancer cells. CAR-T cell therapy is a common immunotherapy treatment for NHL. Bispecific antibodies are a new class of drug treatments that direct your own T cells to eliminate the cancerous lymphoma cells.
Radiation therapy. This treatment uses energy beams from a machine to destroy cancer cells. It may be the only treatment needed for early-stage NHL. Providers also use it to destroy lymphoma cells that remain after chemotherapy.
Chemotherapy with stem cell transplantation. For this treatment, providers give high doses of chemotherapy to treat your cancer. Then, they replace stem cells (immature blood cells) damaged during chemotherapy with healthy ones from your own body or a donor. You may need a transplant if other NHL treatments haven’t worked.
Each treatment has different side effects. Ask your healthcare provider about potential side effects before treatment. They’ll help you weigh the potential benefits of treatment against the possibility of side effects.
What Is the Outlook for Non-Hodgkin Lymphoma?
In some cases, treatment can cure non-Hodgkin lymphoma. This means that treatment has eliminated all cancer cells for good. This is more common after treatment for aggressive B-cell lymphomas. Most aggressive non-Hodgkin lymphomas that come back usually do so within the first two years after treatment, or they never come back. Still, you’ll need regular check-ups so your doctor can check for relapse.
With other non-Hodgkin lymphomas, especially indolent ones, you may have this condition in the long term. This means you may need continuous or occasional treatment for the rest of your life.
It’s important to remember, though, that even when non-Hodgkin lymphoma isn’t curable, current treatments are helping people live longer, fuller lives with this disease.
World Lymphoma Awareness Day 2025—Honest Talk
The 2025 World Lymphoma Awareness Day theme, “Honest Talk,” stresses the vital need for open communication about lymphoma’s physical and emotional impacts. Honest conversations between patients, families, and healthcare providers help manage the stress, uncertainty, and emotional challenges following diagnosis and during treatment. Such openness dismantles stigma, promotes mental well-being, and encourages individuals to access support networks.
TheKnowHow Independent Second Opinion Service
Are you or a loved one under suspect or suffering from lymphoma? You are overwhelmed or unsure about further treatment?
TheKnowHow Independent Second Opinion Service is not intended to take you away from your treating doctor but rather provide an extra level of competence.
Get an unbiased assessment from an international expert without having to travel or schedule appointments. Our impartial specialists conduct a record-based assessment of your current health state and all available treatment options, including their advantages and potential hazards.
Read more on SECOND OPINION MEDICAL
We will be honest. We tell you the facts.
